
Image courtesy of Sanjeevan Kanagalingam
For several decades, people diagnosed with osteoarthritis in a knee would be offered a total knee replacement surgery. Today however, some patients have the option of knee realignment through a High Tibial Osteotomy (HTO), which preserves the native joint by offloading the diseased part and stabilizing it with a titanium fixation plate. Currently, most commercial HTO plates are “one-size-fits-all,” which leads to compromised performance and frequent complications. In the future, patients suffering from knee osteoarthritis may have the option of a biomechanically optimized, patient-specific fixation plate, thanks to the research of University of Birmingham mechanical engineering PhD candidate Sanjeevan Kanagalingam and his research project partners.
Their generatively designed fixation plates for HTO surgery will take into account personalized biomechanical requirements to devise medical-grade titanium alloy implants for matching specific patient needs. Those specifics will include, for example, the shape of the bone, patient weight, joint anatomy, degree of realignment, and typical daily activity levels. This approach offers a tailored solution for athletes who may develop knee osteoarthritis early in life and put their joints through daily high impact levels compared to people with lower activity levels. “With generative design we can tailor those details to each person and create a biomechanically specific design,” Kanagalingam says.
The research team includes the Manufacturing Technology Centre (MTC) in Coventry, UK, orthopedic surgeon Tarek Boutefnouchet, Autodesk Technical Consultant Peter Champneys, and academic supervisors Dr. Lauren Thomas-Seale and Prof. Duncan Shepherd. “This is a unique project in the field of bespoke patient specific knee osteotomy illustrating the perfect product of several years of collaboration between clinicians and engineers,” Dr. Boutefnouchet says. “With increasing longevity, people desire to remain active, fit, and functional at a more advanced age. Joint preserving operations such as knee osteotomy have become crucial in orthopedic surgery. This novel technique will be more precise, accurate, and ultimately will lead to better clinical outcomes.”
From 3D Printing to Generative Design
After earning a master’s degree in mechanical engineering and working as a researcher at the University of Birmingham, Kanagalingam developed a deep interest in 3D printing/additive manufacturing. Then about five years ago, the MTC offered to sponsor his Engineering and Physical Sciences Research Council (EPSRC) National Productivity Investment Fund PhD project, and he began to look at fundamental problems where additive manufacturing could make a tangible difference to patient outcomes, such as orthopedic implants for bone fractures. He eventually narrowed the focus to orthopedic fixations for HTO surgeries.
During his PhD, Kanagalingam won an EPSRC Innovation placement grant, which facilitated a research arrangement with Autodesk, including a course on generative design at the Autodesk Technology Centre in Birmingham, UK. It was there where he met Champneys, who has worked with Kanagalingam throughout his PhD project, assisting with preliminary concepts that eventually progressed into manufactured prototypes that are going into testing and validation. Before linking up with Champneys and Autodesk, Kanagalingam had worked with 3D modeling in Autodesk Fusion 360, but learning about generative design’s AI-enhanced possibilities revealed how Fusion 360 could use multi-faceted biomechanical data to inform patient-specific fixation plate designs. Kanagalingam and Champneys first introduced this novel generative design approach to orthopedic implants at the 2019 Autodesk University Las Vegas.
“With cloud computing and AI based algorithms, we use design requirements like structural stiffness or design for manufacturing to quickly create multiple design possibilities without human involvement,” Champneys says. “This is much closer to nature’s design approach, where each iteration learns and grows from the one before, leading to a final design perfectly suited to its intended environment. And generative design automatically optimizes for the manufacturing method. If additive manufacturing is selected, the algorithm adjusts the shape to reduce the required support material, also reducing post-processing time and cost.”
Throughout this project, Kanagalingam and his collaborators used Fusion 360 for the surgical simulation of the HTO process, defining the surgical parameters for generative designs, and for the detailed final designs of the novel HTO plates. Kanagalingam says the software made it possible to extract those surgical parameters from the 3D models and use them to define clinical requirements for generative design all in one interface.
Proof of Concept Published
Kanagalingam and his research team have published a paper in Progress in Additive Manufacturing (PIAM) that proves the viability of their novel end-to-end workflow including additive manufacturing to produce reliable, patient-specific generatively designed bone fixation devices. This paper’s research was originally presented at the ASTM International Conference on Additive Manufacturing 2021 and represents the most detailed description of generatively designed bone fixation plates thus far in the field.
“The project has been an excellent demonstration of the end-to-end process involved in the generative design, manufacturing, and post-processing of these functional implant prototypes,” says Chris Dalton, advanced research engineer at MTC.
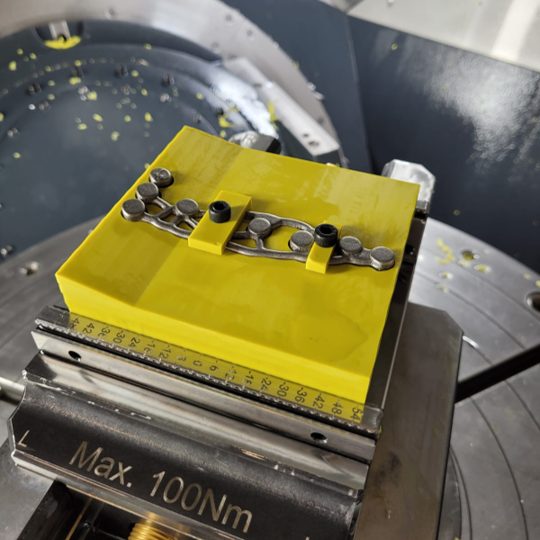
This diverse team of designers, clinicians, and technicians used Fusion 360’s online collaborative features to review the developing iterations of the implant models’ design and manufacturing parameters. When exploring how the implants could be made not only using additive manufacturing methods, but also with CNC machining, they used Fusion 360 to generate the CNC tool paths and machining strategies for manufacturing the fixtures and holes/threads within the implants.
Kanagalingam now has five prototype implants—some made with additive manufacturing and some produced from CNC machining. Next up on the project’s agenda: demonstrating their mechanical performance experimentally. Kanagalingam says they have successfully validated the prototypes computationally, and they could eventually move on to translational clinical testing.
“This generative design approach could be transferable to all orthopedic implants straight away,” Kanagalingam says. “Anything that is load-bearing—not just a knee joint, but also jaw fractures, shoulders—anywhere. I see it being adopted for many reasons. It has opened up the design space for biomedical implants, and I am confident that it will soon be applied by other people in academia and orthopedic industries.”